The FGDP had confirmed recently that it was still their goal to achieve publication of the new guidance notes on the use of x-rays in dental practices by 30 June 2020, following an internal FGDP review process. Having checked on-line today these did not appear to have been put onto the website – but we still feel it is important that you have been made aware of the important changes within the guidance so have decided to send this attachment today.
Please take the time to read it (key area titles are shown in red) and get back to us if you have any questions.
1. HSE
2. Radon
3. RPA or MPE? Roles of Radiation Protection Advisers (RPA) and Medical Physics Experts (MPE) in dentistry.
4. Contingency Arrangements
5. Staff pregnancy
6. What is cooperation between employers and why does it matter to you?
7. Dosimetry
8. Warning Signs & Lights
9. Plans
10. Critical Examination and Acceptance test (CEAT)
11. Rectangular collimation
12. PPE thyroid collars
13. Training
14. RPS Training
15. Inspection Frequency
16. Quality Assurance (QA) ‘subjective image quality assessment’
17. CBCT / Handheld
18. Analogue to digital
19. Disposal of X-Ray Sets
20. Documentation
1. HSE
Under IRR17 dental practices had to register their ‘work with a radiation generator’ with the Health and Safety Executive (HSE). This is a reminder that the registration must be updated if the ownership of the practice changes or you move your practice to a new location. Also has your practice checked there are no ‘classified’ workers shown on the original HSE registration? Dentist and dental staff are not classified workers, this can be updated with the HSE, via the contact me section in your original HSE account. If in doubt – contact SG&A
2. Radon
The dental guidance notes emphasize the need to assess the risk from radon at your practice. Good news – SG&A include this in your updated radiation risk assessment sent with your report. If the risk from Radon in your local area is assessed as above 300Bqm-3 further monitoring will be required and depending on the results you may need to inform the HSE and undertake ways in which to reduce (mitigate) Radon levels. As always, we are here for advice if you need us.
3. RPA or MPE? Roles of Radiation Protection Advisers (RPA) and Medical Physics Experts (MPE) in dentistry.
As a user of a ‘radiation generator’, you must appoint a suitable RPA under IRR17. You must seek the RPA advice for at least the following areas:
• Prior assessment of plans (before work commences) for new or modified practices/rooms.
• Acceptance into service (e.g. assessment of engineering controls, design features, safety and warning devices) for new or modified radiation sources – e.g. changing from a panoramic (opg) unit to a cone beam ct unit. This includes CEATs.
• Designation of controlled and supervised areas and subsequent requirements
• Periodic testing of engineering controls, design features, safety and warning devices and the regular checking of systems of work (e.g. your local rules)
For dental radiography an appropriate MPE must be consulted on ‘employers procedures’ required under IRMER17, the ‘optimisation of patient doses’ (keeping the doses to patients as low as reasonably practicable) and the acceptance testing of dental X-ray equipment. MPEs also give advice on dental X-ray and ancillary equipment (eg, digital image receptors, phosphor plates, etc), the application and use of diagnostic reference levels, optimisation of doses to patients and others (such as carers and comforters) and advising employers regarding compliance with IRMER17. The RPA and the MPE appointed may be the same person as long as they have RPA2000 RPA certification and are also ‘listed’ as an MPE by RPA2000.
As your RPA and MPE we are here, so If in doubt – as always please shout!
4. Contingency Arrangements
What happens if something goes wrong? Do you know what the contingency plans are for your practice? Essentially switch the power off to the x-ray unit? Absolutely – it is important to know your contingency arrangements and show they are ‘rehearsed’ (annually).
The new guidance notes require a formal investigation into the circumstances surrounding any incident when contingency plans are used.
‘Significant Accidental or Unintended Exposures (SAUE)’ replaces the concept under IRMER2000 of doses that were ‘much greater than intended (MGTI)’ and introduces a specific dose level of 3mSv.
5. Staff pregnancy
The words radiation and pregnancy used together can make people nervous, so It is important employers and staff discuss concerns.
SG&A advice with regards to pregnancy? Female employees must be informed of the importance of notifying their employer as soon as they are aware of their pregnancy. The radiation protection of the foetus is the expectant mothers responsibility until the employer is notified. We recommend this exchange of information is done in writing. When the employer is aware of the pregnancy, they are required to ensure the dose to the foetus will not exceed 1 millisievert for the remainder of the pregnancy and putting it in writing sets the start date.
It is important to remember local rules are primarily designed to keep doses ‘as low as reasonably practicable’ and ALL staff and operators must comply with these. Normally no changes to working practices of the pregnant staff member are required. We recommend reissuing the local rules to pregnant staff to read and they should then sign and date the local rules agreement form to indicate this has been done. SG&A provide our clients with updated radiation risk assessments to include pregnancy aspects so normally this requires no further action.
When SG&A complete a site visit, we undertake dose rate surveys and measure scattered doses at the operator positions. This is provided in your report, along with any shielding recommendations. This can be used to reassure staff they are safe as long as they work within the Local Rules.
Information for staff regarding pregnancy can be found in the pregnancy procedures section of the local rules.
As a reassurance measure personal dosimetry can be issued to the staff member for the remainder of the pregnancy. This is not a legal requirement but may well provide piece of mind to the expectant mother and/or employer. SG&A can provide dosimetry services – please contact us for further information.
6. What is cooperation between employers and why does it matter to you?
Any other ‘employer’ conducting work on your x-ray devices (e.g. RPA/MPE, installers, service engineers) needs to complete a ‘handover’ of the controlled area from and back to the practice. This is generally a form which documents that you have ‘released’ control to the other employer and then they have given you back this control indicating that the units are working appropriately. Any ‘handover form’ should be signed by both parties and make sure you have a copy retained for your records.
7. Dosimetry
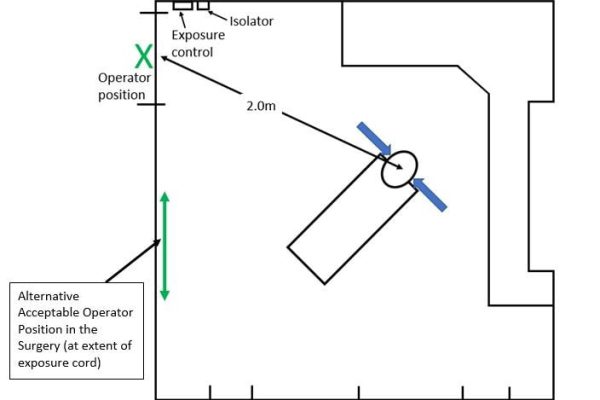
Because of the requirements in the IRR17 the Health and Safety Executive (HSE) have indicated that they will no longer accept ongoing ‘calculated’ assessments of doses to operators and any other non-classified persons who enter or might enter controlled areas within dental practices. As this is to confirm that the surgery/imaging room local rules for your practice are effective in restricting exposure the expectation is that these measurements should be undertaken using personal dosimetry or other ‘suitable means’ such as environmental dosimetry – with dose rate surveys (such as those SG&A carry out in your practices when we visit) confirming levels of dose in operator positions and through walls to confirm appropriate levels of shielding.
The use of dosimetry in practices does not have to be long-term but is expected for the initial use of a hand-held dental x-ray unit, should be undertaken for new practices and equipment and also considered for pregnant staff and changes in workload. The use of dosimetry and dose rate surveys should be reviewed with your RPA – and do be aware that there are now different types of dosimetry – such as the Mirion Instadose – which no longer have to be returned to the supplier periodically (e.g. every three months). Please do not hesitate to contact us for more information.
8. Warning Signs & Lights
As you designate ‘controlled areas’ in dental x-ray imaging you will now definitely need to have warning signs. They should be visible at each entrance of the controlled area (e.g. the surgery room) – and now this includes any entrance where the operator stands. Signs need to include the ionising radiation trefoil symbol and wording to include ‘X-rays’ and ‘controlled area’ (and perhaps ‘no unauthorised entry’). The controlled area is to be ‘designated’ when unit is switched on.
Warning lights can be considered but are not needed if operator can easily control access to the room or access can be restricted for example through locking a door (so they are not needed for a cone beam CT room with one entrance that the operator can control). If warning lights are used they must be accompanied by a notice explaining the significance of the light and should be connected in such a way that they illuminate automatically when the unit isolator is turned on (that is while the X-ray set is in a state of readiness to emit X-rays).
9. Plans
Did you know an RPA must be consulted to undertake a prior examination of plans? We give you practical advice on the radiation protection aspect of plans. Installing companies are becoming more diligent in reminding owners an RPA needs to inspect plans but please remember it is technically your responsibility to ensure this has been done (HSE and CQC will check this at inspection visits). Please don’t hesitate to contact us for further advice.
10. Critical Examination and Acceptance test (CEAT)
What is a Critical Examination and Acceptance test (CEAT)? When do I need a CEAT? How often do I need a CEAT?
A CEAT or Critical Examination and acceptance test ensures a newly installed, relocated or repaired x-ray unit is safe, operates correctly, and people are not at risk from ionising radiation.
The installer is responsible for ensuring the ‘critical examination’ of the unit is conducted for all X-ray units. The examination should be carried out as soon as possible after installation and the equipment should not be used until written confirmation has been received that it provides adequate protection.
The acceptance test is the responsibility of the employer under IRMER17. Adequate testing must be completed on X-ray equipment before it can be put into clinical use. The purpose of this is to confirm that the equipment is operating correctly and is capable of the adequate restriction of patient dose. Often the acceptance testing is conducted at the same time as the critical examination, however; if this is not the case the employer should consult its MPE (SG&A) regarding alternative arrangements.
A CEAT is required for:
1. a newly installed x-ray unit
2. if a major component is changed such as a timer or tube head
3. if the unit is moved within a surgery or a different location.
Critical examinations and acceptance testing are not carried out every 3 years (this is called ‘routine’ testing). There should be a CEAT for every x-ray unit on site, which must be retained and available to present to the CQC or HSE. If a CEAT cannot be found for an x-ray unit on site the practice has two options:
1. Contact the original installer and ask for a copy if the original paperwork (depending when installation was).
2. Have a ‘retrospective’ CEAT conducted – SG&A can provide this service, please contact us for more information.
Just to clarify, the term ‘critical testing’ or ‘performance testing’ do not refer to CEATs although the wording suggests they do.
11. Rectangular collimation
Why use rectangular collimation? What does the updated guidance say about rectangular collimation?
Rectangular collimation reduces the effective dose to the patient (and the scattered dose to staff) – by a good 40% or more compared to the old circular collimators. This means it should always be used for periapical, bitewing and occlusal radiography, unless there are sound clinical reasons for not doing so (essentially where the use of that rectangular collimation ‘would’ (not could) lead to a high number of repeat exposures). If the use of circular collimation is considered justified (consult with your SG&A MPEs on this) this – with the reason – needs to be documented in the patients notes following.
The new guidance also states rectangular collimation is to be provided as standard on all new intra-oral x-ray units and for equipment that is still fitted with a circular collimator, a rectangular adaptor/insert must be provided. The size of the collimator should be no greater than 40 mm by 50 mm, and preferably less than 35 mm by 45 mm – and rectangular collimation should be used with beam aiming devices and image receptor holders for periapical and bitewing radiography wherever clinically possible. This will improve image quality and reduce the number repeat exposures.
12. PPE thyroid collars
One question we at SG&A often encounter is regarding the use of thyroid collars. The simple answer is there is still not any general requirement for the use of a thyroid collar during dental imaging – unless the thyroid gland is going to be in the main beam. If this situation is likely then the use of a thyroid collar should be discussed with an MPE.
13. Training
Under IRR17 and IRMER17 it is the responsibility of the employer to ensure anyone involved with dental X-ray exposures is adequately trained for their role. Training must incorporate theoretical and practical aspects. There must be continuing education and training of verifiable CPD in radiation protection and radiology in each five-year CPD cycle.
Training with regards Cone Beam CT (CBCT) units is split into a two tiered system – Levels 1 and 2. Level 1 is broken down into Operators level 1 for dentists and dental nurses who use the units, or a Referrers level 1 for requesting CBCTs. Level 2 is required to be able to diagnose from CBCT images. For CBCT trained staff it is suggested a minimum of one hour of the recommended 5 hours of verifiable radiation protection/radiology CPD should be specific to dental CBCT.
Users of Handheld x-ray devices must complete relevant training to successfully utilise the units integral shielding, only use as near horizontal X-ray beams as possible and use the appropriate beam aiming devices and image receptor holders.
Most importantly remember to document your levels of training in your Radiation Protection File!
14. RPS Training
What does the RPS do? The RPS helps to ensure legal compliance with the Ionising Radiation Regulations 2017 (IRR17). They should be your first contact if you have any concerns and if you need further help or guidance contact us! Radiation Protection Supervisor must be ‘appropriately and adequately’ trained and undertake refresher training between 3 and not exceeding 5 years. A copy of the certificate to show this training has been completed should be in the Radiation Protection File. The RPS should be listed on the Radiation Protection documentation for your practice. The RPS must be appointed in writing by the Employer and a copy of the appointment letter kept in the Radiation Protection File.
15. Inspection Frequency
What do you need to have checked and when in relation to your x-ray devices? It can be confusing with the different terminology used to know what you need to have done and when and what are the Legal requirements?
1. Legally a CEAT must be conducted on all x-ray units at installation, if the unit is relocated or a major component replaced (see the earlier section in this newsletter).
2. ‘Routine’ (radiological) testing should be conducted at appropriate intervals – that is at least once in a three year period or more often if necessary (e.g. if reference levels for imaging are too high) for intra oral x-ray units, annually for CBCT and handheld units. This testing (also known as ‘equipment performance’ testing) is carried out as part of your assessment visits from SG&A.
Please note that the new guidance notes indicate that CBCT units require annual testing, except where there is no performance specification or QA test object available from the manufacturer, or these have not been provided.
3. Servicing must be conducted according to manufacturer’s recommendations by an appropriate x-ray engineer – this is generally annually – of the x-ray units at the practice. This should include general electrical and mechanical maintenance only (not routine testing as well with SG&A as your RPA/MPE).
**FILM PACK TESTING IS NOT REQUIRED ** – you would simply be paying for the same work being carried out twice as we measure radiological output at the time of our visit). Please get in touch if you are at all unsure about your need for testing.
16. Quality Assurance (QA) ‘subjective image quality assessment’
One big change that has come about with the new guidance notes is the revised image quality rating and analysis grading. Due to increased use of digital imaging systems a new two-tier grading system has been introduced. Images are now to be rated either as a grade 1 (an acceptable image) or grade 2 (unacceptable image), rather than grade 1, 2 or 3.
Grade one is defined as ‘No errors or minimal errors in either patient preparation, exposure, positioning, image (receptor) processing or image reconstruction and of sufficient image quality to answer the clinical question’.
Grade two is defined as ‘Errors in either patient preparation, exposure, positioning, image (receptor) processing or image reconstruction which render the image diagnostically unacceptable’.
For digital imaging systems a target of not less than 95% grade 1 and not greater than 5% grade two has been set, this changes to not less than 90% grade 1 and not greater than 10% grade two film systems. It is really important that the ‘minimal errors’ (e.g. cone cutting, slightly incorrect positioning) are documented so that when you audit these results you can look at ways to correct these issues (e.g. in-house discussion/teaching) and improve your future images and target scores.
17. CBCT / Handheld Unit Guidance
Good news! The previous CBCT and handheld guidance has been updated and incorporated into the new ‘Dental Guidance Notes’ – all your compliance needs in one (larger ?) document.
18. Analogue to digital
Thinking of going digital…. If your practice is moving from an analogue film system to a digital film system, then please contact us. As your MPE we give you advice on updating your x-ray settings for your new system – as required by the IRMER regulations and indicated in the guidance notes.
19. Disposal of X-Ray Sets
The employer is responsible for the disposal of the x-ray set with regard to radiation safety – this can be achieved by removing the electrical power cable (once disconnected) and removing / obscuring trefoil symbols or other ionising radiation hazard indicators.
Dental x-ray devices are not exempt under WEEE regulations and as such the employer has to consider their duties under the Waste Electrical and Electronic Equipment Regulations 2013 (WEEE) and the Special Waste Regulations 1996. If you use a contractor to dispose of your waste it is your responsibility to ensure the contractor has the appropriate paperwork.
In most cases if you are having a new unit the installer will offer a disposal service – or you can contact the original installer or manufacturer for advice.
If you are selling or gifting an x-ray set the employer selling or transferring the dental X-ray equipment has the same obligations to pass on adequate information to the new user regarding the safe use, testing and maintenance of the equipment as would the original supplier.
20. Documentation
Lastly, one question here at SG&A that we are often asked is how long do I have to keep records for? For clarity here is a summary:
Document Retention Period
HSE Registration – Until registration is changed or cancelled
Radiation risk assessment – Until superseded by updated version
Local Rules – Until superseded by updated version
Record of critical examination – Working life of the X-ray equipment
Personal dose monitoring of non-classified employees – At least two years
Report of dose investigation level (but not dose limit) exceeded – At least two years
Investigation of contingency plans being used – At least two years
Monitoring of controlled areas – At least two years
Maintenance and examination of engineering controls – At least two years after subsequent test
Checks of safety and warning features – At least two years after subsequent test
Examination of PP – At least two years after subsequent test
Records of staff training in radiation safety – At least five years
Controlled area hand-over forms – At least three years
Thank you for taking the time to read this as always if you have any questions or queries as your RPA and MPE we are here, so If in doubt – as always please shout!
S. Green
Principal RPA, RWA & MPE Stephen Green & Associates Ltd.